Article
10 min read
Is there a need for a hospital reference architecture plan?
Is there a reference architecture for hospitals in Hungary? Since we can find no trace at all of any hospital reference architecture plan in our country, we conclude that none exists. If it does exist, it has been successfully hidden, so, unfortunately, it cannot fulfil its function. Anyone missing it? Do we need it? Although we cannot find a domestic answer, there are known attempts at international level.

But what is a reference architecture plan and what is its purpose?
There is a growing social demand and social willingness to improve health services. Change is ongoing (reform of the health care system, including plans for primary care, outpatient care, laboratory networks, etc.), with wide-ranging impacts that affect hospitals in different ways. This is due, among other things, to the lack of uniformity in the way institutions are organised to operate, and the systems that support them to meet legal requirements are not uniform either.
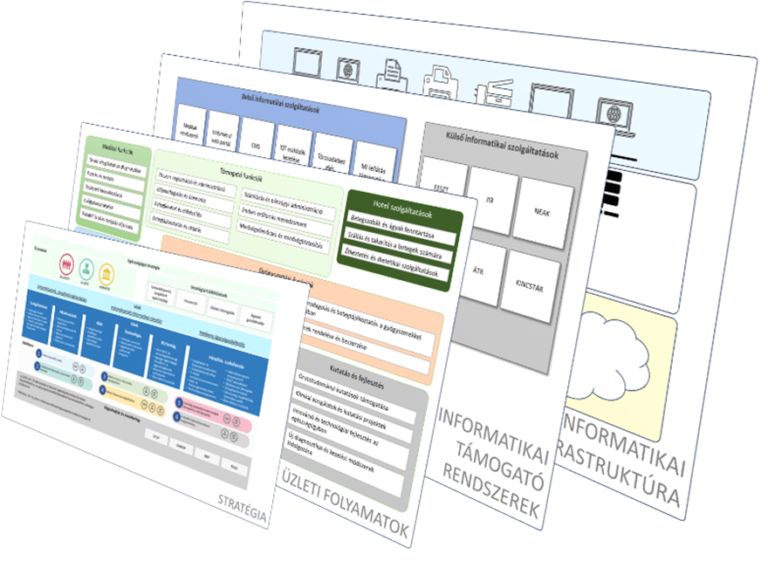
A reference architecture is a planning template or pattern that describes the ideal architecture, design principles, and recommended practices for a given system, application, or service. A branch or sector-specific reference architecture, also known as a reference model, serves as a guide or template for the "architects" of an organisation, who can tailor it to the characteristics of their own organisation.
One of the great advantages of reference architectures is that they contain reusable architectural elements, be it a function (e.g. care service documentation, electronic fever charting, prescription writing, etc.) or a process (e.g. patient management, nursing care, medication supply). These building blocks have the characteristic of having well-defined boundaries and interfaces, forming part of the common body of knowledge that can be reused again and again.
The health sector is facing major changes. A reference architecture can always serve as a model and base map for the sector management, hospitals, and the companies providing services to hospitals. How? Consider for instance the case when the sector management decides to change an element of health care (e.g. outpatient management, remote diagnostics, or telemedicine services). With a hospital architecture plan, it is much easier to model the impact of the intended changes based on the reference architecture, and simple to determine which other building blocks will be affected, where and how modifications should be made to them.
What is the current situation in Hungary?
Our domestic hospital informatics must overcome very similar problems as many other European countries. Health informatics, no matter how wide open the gates of technological opportunities are, must jump further steps ahead and find its properly appreciated place.
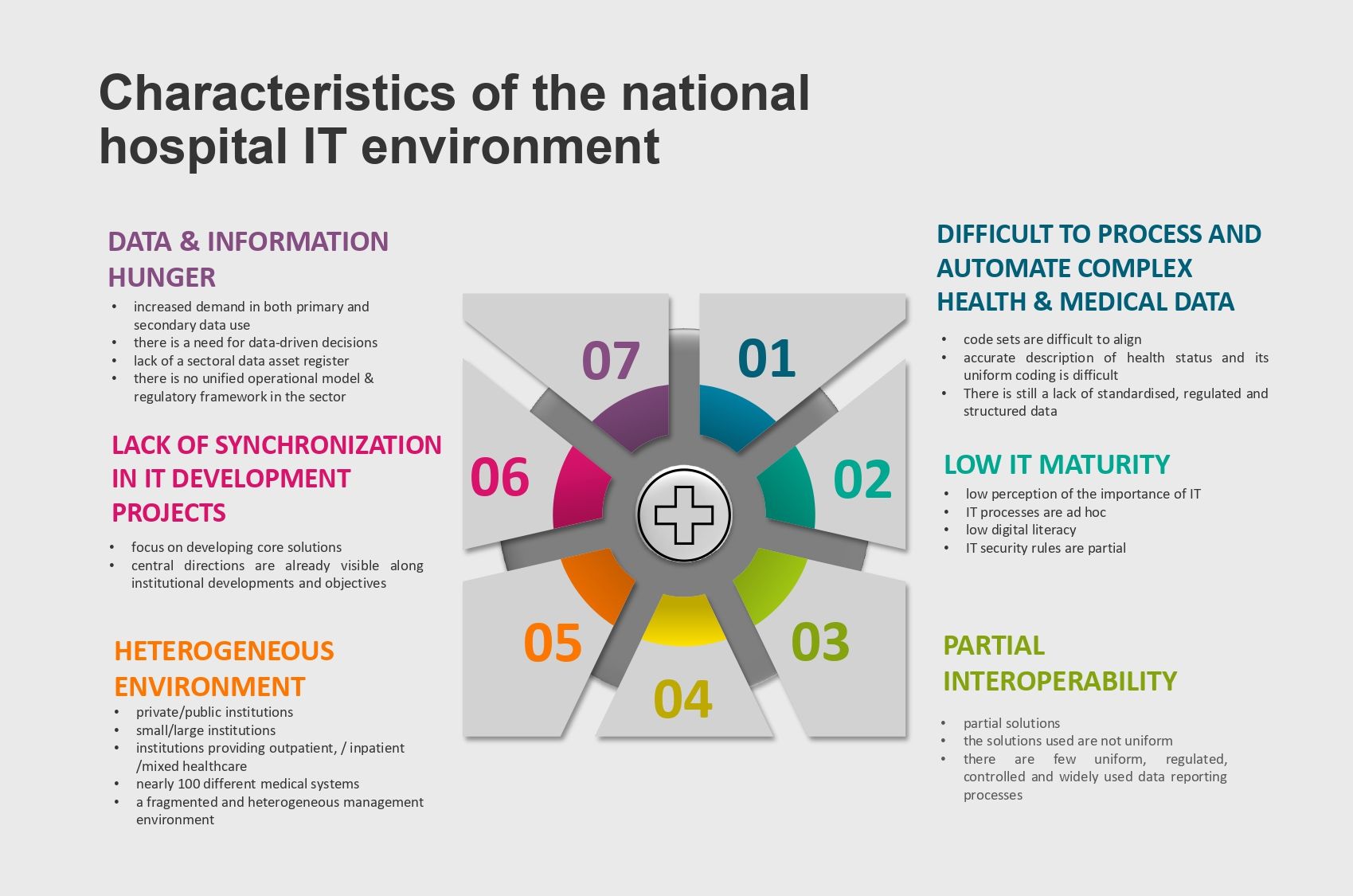
Heterogeneous environment
The number and diversity of medical systems have grown over the years. This is exacerbated by the fact that the systems produced are not based on a common data model, which foreshadows the problem of interoperability or rather non-interoperability. These systems have provided/provide solutions to different areas of healthcare, sometimes better, sometimes worse, and sometimes in a truly excellent manner, building on many working hours of engineering and development. Everyone had to come up with much the same thing, but the answers and solutions were inevitably different.
Low IT maturity
Despite an improving trend in recent years, the perception of the importance of IT is still low. The sector faces many challenges on a day-to-day basis, and the daily provision of care is more of a painful spot for institutions than the delay in exploiting the potential of IT.
Departments have been set up within the organisations of institutions to deal with IT tasks; however, their operation and the processes they use are often incidental. They rely or depend more on personal expertise and knowledge than on documentation and controlled operations.
Unfortunately, the digital literacy of a wide range of health workers is low. As a result, understanding and using IT, IT solutions and toolkits can sometimes be quite cumbersome.
Interoperability
In the health sector, a number of data connections have been developed in recent years. Some of these links were established in a centrally imposed, regulated way, others are based on some commonly agreed standard communication protocol (e.g. between two institutions on HL7 basis), or on a vendor-supplied (e.g. PACS) system typically using standard interfaces. Although these connections are based on standard or internationally accepted recommendations, they are not uniform. When implementing a new connection, major interface matching challenges arise, and the data categories and formats transmitted through the interfaces are again not always uniform.
Therefore, uniformly defined data are important to allow for the interpretation and comparison of information for both primary and secondary data use. This is the case, for example, when a doctor compares a patient's laboratory results (primary) or a researcher compares the reports of several patients (secondary) and draws conclusions. Finding and applying a common language is essential for interpreting the data.
Health and medical data are complex and difficult to process
All disciplines, including healthcare, are convinced that their own particular tasks and activities are the most complex and most intricate things in the world, so to describe, standardise and restrict them with frames is almost impossible. Healthcare is no different. Many legislative rules, regulations, recommendations, international and national standards set out how and where the persons involved in healthcare should carry out their tasks. and what data and information they should record and use.
In the health sector, considerable knowledge, content, and technical solutions have been developed over the years and decades at the individual back office institutions (NEAK, NNK, OGYÉI, OKFŐ) and the various actors in the sector. These data, the structure and semantics of the data have been developed and implemented in the different sectoral systems according to the best knowledge of the fields concerned. Several central data masters and registers have been put in place (thanks to legal requirements) and adopted by the sector. However, there is still a need for the precise definition of data, data elements, and the introduction of central code sets and data masters that unify the use of healthcare services and individual sectorial data.
However, uniform data capture will only be of value if the data transfers also become widely regulated and structured.
Lack of coordination of IT developments
Development basically takes place in two different ‘workshops’. In one, institutional improvements are identified and, if resourced, implemented, while in the other, central systems are developed which, in one way or another, are extended to many other institutions in the sector. This in itself would not be a problem, but in many cases, the solutions to local and central objectives are not necessarily aligned or harmonised with each other, or do not take account of the development needs, plans, or specificities of the other area.
Not all development can or should be centrally managed, but it is necessary to set out strategic principles and directions and to ensure that they are followed.
Data and information hunger
There is a growing demand for data in relation to services directly related to healthcare processes and activities, as well as in the supporting economic, logistics, and other background processes, local and sectoral management, and in scientific, research, or teaching activities. The need for data-driven decision-making is growing and there is increasing demand for data-based technologies that allow automation or even artificial intelligence-assisted decisions.
The healthcare sector is sitting on top of huge and valuable data assets with elements without a comprehensive or detailed picture. There is no single central register of sectoral data assets and their components. The data stored in various systems and their data content exist as part of distributed knowledge systems.
There is a need for a unified sectoral operating model and a system of rules that covers the definition of rules and recommendations of both existing and future IT systems. There is a need for a body or organisation responsible for data management in the sector.
About authors

Zoltán Tim has been working in the field of information security, IT and security management systems for 26 years. In this context he has developed IT architectures for domestic and international companies, typically to increase operational efficiency, security and compliance. He has experience and certifications in audits, risk management, compliance, strategy development, process organisation, regulation, system implementation.

György Lokodi has been working in health informatics for more than 10 years. He participated in the establishment and implementation of the Electronic Health Services Space (EESZT), developing accreditation methods for connected systems, conducting system assessments, and implementing or replacing IT systems in multiple hospitals.